HMS Graduate Program
Mailing Address
Cleveland State University, Washkewicz College of Engineering
2121 Euclid Ave., WH 305
Cleveland, Ohio 44115-2214
Campus Location
Washkewicz Hall Room 305
2300 Chester Avenue
Phone: 216.687.3954
nrt@csuohio.edu
Web Only Contact
Phone: 216.687.3954
nrt@csuohio.edu
Implantable Devices and Regenerative Medicine
Overview
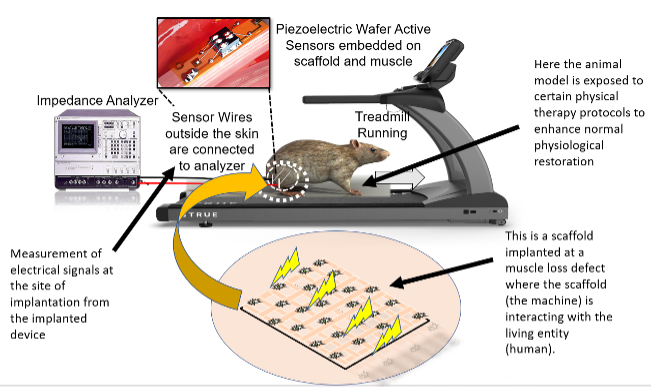
This IKTeam's long-term objective is to develop and validate therapeutic devices that treat physiological defects at a cellular and tissue level. The defects could be bone, muscle or spine-related resulting from trauma or pathological reasons. The devices will be developed using conventional tissue engineering techniques or state-of-the-art bioprinting and 3D printing. Specifically, the devices will be engineered to regenerate the physiological defect and restore normal tissue/organ function. This IKTeam's primary focus is on the individual of the IET framework but also explores how the individual undergoing the therapy interacts with the environment. In addition, the effect of specific physical interactions like walking, running, or routine physical therapy might have on the individual who has been engrafted with a medical device. Understanding individual-environment interactions might help us develop treatment strategies whose therapeutic efficacy can be maximized by synchronizing them with daily activities like walking or running.
Example Projects
Project 1: ‘Design-Specific' and ‘Patient-Specific' Piezoelectric Devices for Bone Regeneration
There is substantial evidence in the literature that clinical electrical stimulation helps in bone regeneration and fracture healing. It has also been proven that piezoelectric implants capable of generating in-situ electrical fields can help bone regeneration. However, no studies have developed piezoelectric implants specific to the bone defect architecture and their corresponding anatomy. Hence, the primary object of this research project is to develop defect- and patient-specific piezoelectric implantable devices for treating bone fractures resulting from trauma or bone diseases (like osteoporosis). The present project challenges us to find answers to questions like ‘How well can we optimize device design and performance?', ‘How can we strengthen the interaction of implantable devices with patient-specific anatomy to maximize restoration?', ‘What are the short and long-term performance characteristics of the device in gradually changing bone morphologies?
Project 2: Smart nano-therapeutic device for on-site elastic tissue regeneration in musculoskeletal disorders ( Faculty: Kothapalli, Sikder, Yu)
Elastic fibers are the primary component responsible for providing tissue flexibility. In case of degenerative disorders or injury, these elastic fibers fail to naturally repair or regenerate, leaving a stiff extracellular matrix (ECM) for the tissues. This dysfunction falls under the family of ‘proteolytic disorders' and includes various pathological conditions such as psoriasis (skin), emphysema (lungs), irritable bowel syndrome (gastrointestinal), rheumatoid arthritis (auto-immune), and aneurysms (vascular). The central theme of this project is to develop a nano-therapeutic device that will be able to interact at a sub-cellular level and enhance in-tissue matrix repair. These nano-devices will help regenerate elastic fibers in the context of skeletal muscle disorders. We call these ‘smart' as these nano-devices are programmed to target the injured site and perform the therapeutic action required to regenerate the elastic fibers. In this project, the investigators want to go a step ahead and engineer these nano-device systems so that it helps with in-tissue matrix repair in the context of musculoskeletal disorders.
Members
Prabaha Sikder

Prabaha Sikder is an Assistant Professor in the Department of Mechanical Engineering and a faculty at the Center for Human-Machine Systems. His research focuses on the development of state-of-the-art technologies, especially biomaterials for tissue regeneration. He develops medical implants and scaffolds which aim to treat orthopedic and musculoskeletal defects. Some of the solutions developed by him include antibacterial coatings, biodegradable bone-grafting materials, and 3-D printed bioactive polymer-ceramic scaffolds.
Ph.D., Mechanical Engineering, University of Toledo, 2019
M.S., Production Engineering, West Bengal University of Technology, 2015
B.S., Mechanical Engineering, SRM University, 2013
Chandrasekhar Kothapalli

Dr. Kothapalli built a research program at the interface of engineering and medicine, with strong clinical applications in regenerating diseased or injured tissues and organs. He integrates his background and expertise in stem cells, tissue engineering, biomaterials and nanotechnology to develop long-lasting solutions for vascular and neural clinical conditions.
Ph.D., Bioengineering, Clemson University, 2008
M.S., Materials Science & Engineering, University of Connecticut, 2005
M.S., Chemical Engineering, Mississippi State University, 2002.
B.S., Chemical Engineering, Andhra University, India, 2000
Josiah Sam Owusu-Danquah

Dr. Owusu-Dabquah is an assistant professor at Civil and Environmental Engineering Department at CSU. His research focuses on computational mechanics, material modeling, testing and finite element simulation of stimulus-responsive materials and devices. He has also worked on simulation of shape memory micro actuators, biomedical self-expanding stents and nitinol bone staples.
Ph.D., Civil Engineering, The University of Akron, 2017
M.S., Civil Engineering, Southern Illinois University Carondale, 2013.
B.S., Civil Engineering, KNUST, Ghana, 2008
Anne Su

Dr. Su's primary background and research interest is in biomechanics. Dr. Su gained experience in medical device design, spinal biomechanics and implant design, ergonomic design, and human movement analysis. She also helped to develop computational models of human and animal movement for application in studies of injury mechanism.
Ph.D, Physical Anthropology, Stony Brook University, 2011.
M.S., Mechanical Engineering, University of Michigan, 1999.
B.S., Mechanical Engineering, Case Western Reserve University, 1997
Deborah d Espy

Deborah Epsy's areas of clinical expertise within Physical Therapy are neuro-rehab, assistive technologies, seating and mobility, acute care, and geriatrics. Her research interests are in the areas of motor learning, postural control and falls, and off-the-shelf technology for rehab and health, and knowledge translation for rehab technologies.
Ph.D., Movement Science, University of Illinois at Chicago, 2010
M.S., Physical Therapy, Medical College of Virginia and
Virginia Commonwealth University, 1992
B.A., Biology/Pre-Physical Therapy, College of Wooster, 1989
Mailing Address
Cleveland State University, Washkewicz College of Engineering
2121 Euclid Ave., WH 305
Cleveland, Ohio 44115-2214
Campus Location
Washkewicz Hall Room 305
2300 Chester Avenue
Phone: 216.687.3954
nrt@csuohio.edu
Web Only Contact
Phone: 216.687.3954
nrt@csuohio.edu