Department of Electrical and Computer Engineering
Contact
Mailing Address
Cleveland State University, Department of Electrical and Computer Engineering
2121 Euclid Ave., FH 332
Cleveland, Ohio 44115-2214
Campus Location
Fenn Hall Room 332
1960 East 24th Street
Phone: 216.687.2589
Fax: 216.687.5405
ece@csuohio.edu
ECE News 2024
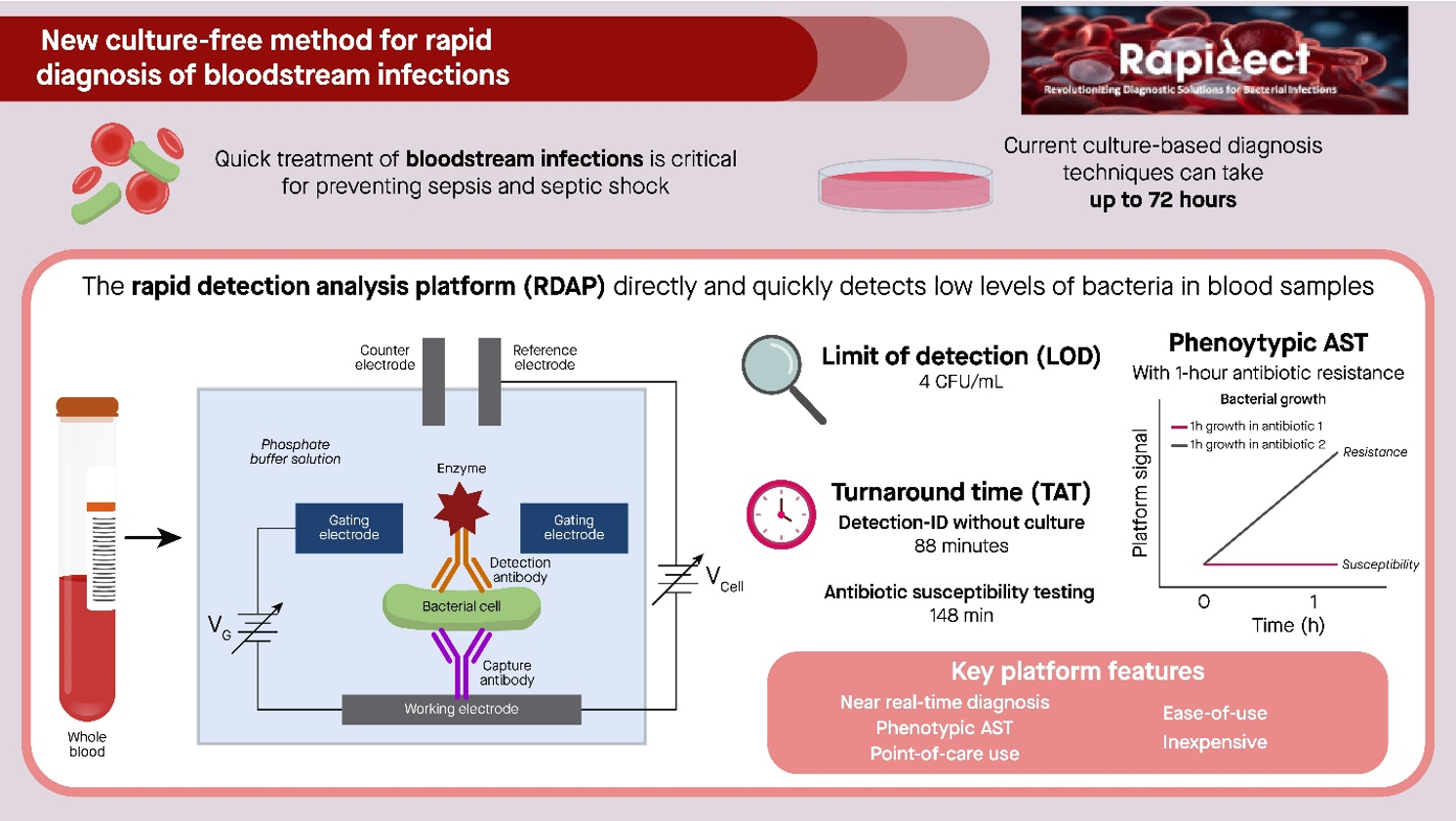
CSU-UM team has demonstrated near real-time diagnosis of bloodstream infections
According to WHO, bloodstream infections (BSIs) remain some of the most common causes of death due to its tendency to cause sepsis. It is projected that, if no action is taken now, BSIs will lead to 10 million deaths worldwide by 2050. The current gold-standard diagnostics for BSIs are based on bacterial culture. The usual culture time of blood is 16-48 hours, making the time-to-result of the diagnosis as much as 74 hours or longer. An unmet need in the treatment of BSIs is providing targeted treatment using narrow-spectrum, bacteria-specific antibiotics that are desirably initiated in the very early stage of infections. Such treatment depends on the availability of diagnostic technologies that provide rapid diagnosis. Current diagnostics for BSIs require positive culture as an input and therefore are subject to the delayed time-to-result.
In a recent news release from the Weil Institute for Critical Care Research and Innovation of the University of Michigan, a platform that provides near real-time diagnosis of BSIs is described together with a study on a cohort of clinical blood samples using the platform. A collaborative effort between Cleveland State University and the University of Michigan, this pilot study was conducted in the previous Clinical Microbiology Lab of the Saint Vincent Charity Medical Center in Cleveland, Ohio and supported by NSF via the start-up company Rapidect. The Rapid Detection-Analysis Platform (RDAP) is an electrochemical immunoassay platform with intrinsic signal amplification. The RDAP allows the direct detection of extremely low-concentration bacteria in blood samples without culture. As such, the RDAP provides near real-time diagnosis of BSIs.
The results of this study were recently published in Communications Medicine. In this paper, the team reports a comparison of the clinical performance of the RDAP with that of standard culture-based microbiology testing methods using blood samples obtained from patients at the Saint Vincent Charity Medical Center. The cohort of 56 samples consisted of both positive culture as well as negative culture samples. The positive culture samples included a range of typical bacteria that cause BSIs. In this study, the RADP achieved a diagnostic accuracy of 93.3% and 95.4% for detection-identification and antibiotic susceptibility testing, respectively. However, the RADP results became available at least 16 hours earlier than those produced by the standard lab methods.
“RDAP needs 88 minutes to perform the detection-identification step. Considering the 16-plus hours required by the standard lab procedure for this step, RDAP is already a near real-time diagnostic for the screening of specific bacterial species,” said Dr. Siu-Tung Yau, a Professor of Electrical Engineering at Cleveland State University and the inventor of RDAP.
The team envisions that, by using RDAP to expedite time-to-diagnosis, it will also bring about a reduction in the use of broad-spectrum antibiotics at hospitals and could decrease patients’ overall length-of-stay and hence the cost of treatment. “What we hope is to reduce the dosage of broad-spectrum antibiotics that our patients are receiving,” said Dr. Scott VanEpps, an MD in emergency medicine at Michigan Medicine and an associate professor of emergency medicine and biomedical engineering at UM. “With near real-time diagnosis, they may only have to receive one dose before transitioning to targeted therapy, whereas right now they typically receive anywhere from 4-10 doses. Additionally, many of these antibiotics can only be administered through an IV. But by transitioning to oral antibiotics earlier, we can help patients leave the hospital sooner.”
The team is currently focusing on using RDAP to achieve near-real-time screening of a small group of bacteria that are notoriously known to cause BSIs in the hospital environment. Among these bacteria is methicillin-resistant S. aureus, which is responsible for a large fraction of hospital-acquired infections. This project is being carried out in the Clinical Microbiology Lab of University Hospitals in Cleveland. It is expected that the outcomes of this project will effectively facilitate antimicrobial de-escalation, which is a component of antimicrobial stewardship aimed to reduce exposure to broad-spectrum antibiotics, by limiting the use the antibiotics to only one dose.
As a final note, compared with polymerase chain reaction, a mainstream molecular diagnostic technology, RDAP is a potentially low-cost detection-analysis technology with ease-of-use and point-of-care compatibility.
Studies Referenced
Shi, X., Sharma, S., Chmielewski, R.A. et al. Rapid diagnosis of bloodstream infections using a culture-free phenotypic platform. Commun Med 4, 77 (2024). https://doi.org/10.1038/s43856-024-00487-x
Shi, X., Kadiyala, U., VanEpps, J.S. et al. Culture-free bacterial detection and identification from blood with rapid, phenotypic, antibiotic susceptibility testing. Sci Rep 8, 3416 (2018). https://doi.org/10.1038/s41598-018-21520-9
S.-T Yau and J. S. VanEpps, A novel way to perform rapid diagnosis of bloodstream infections, Springer Nature Research Communities, https://communities.springernature.com/posts/a-novel-way-to-perform-rapid-diagnosis-of-bloodstream-infections?channel_id=behind-the-paper
Contacts
Siu-Tung Yau: s.yau@csuohio.edu, syau@rapidect.com
J. Scott VanEpps: jvane@med.umich.edu
Contact
Mailing Address
Cleveland State University, Department of Electrical and Computer Engineering
2121 Euclid Ave., FH 332
Cleveland, Ohio 44115-2214
Campus Location
Fenn Hall Room 332
1960 East 24th Street
Phone: 216.687.2589
Fax: 216.687.5405
ece@csuohio.edu